(By Namini Wijedasa/ Sunday Times)
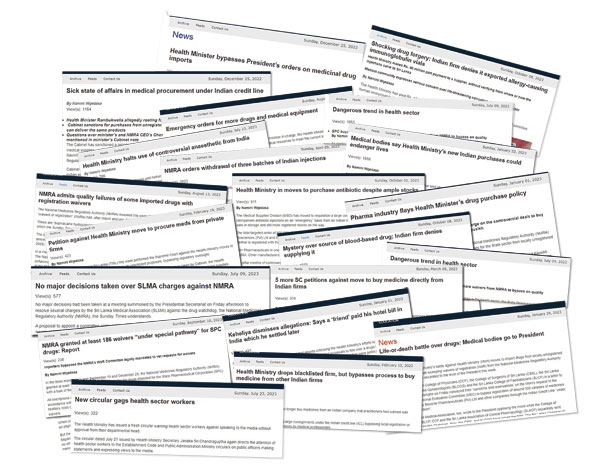
Below are just some of the transgressions highlighted in the National Audit Office’s (NAO) 887-page report.
Cabinet bypassed
In June 2022, the Finance Ministry Secretary directed the Health Minister to submit a report of purchases made under the special “Health Sector Emergency Procurement Process” (HSEPP) for covering approval of the Cabinet every month, along with justifications. Cabinet sanction had not been obtained even up to March 31 for procurements worth US$ 20 million and 633 other emergency purchases valued at Rs. 22 billion made between June 2022 and November 2023.
In September 2022, a decision was made at a meeting between the then Health Minister and medical suppliers to import three months’ worth of “vital and essential medicine” under the Indian credit line (ICL).
On the instructions of an Additional Secretary to the Ministry of Health—who is now in remand custody—expressions of interest (EoI) were drafted for 285 medicines and submitted for the Health Secretary’s approval. The list included non-essential items passed off as emergency requirements.
The EoI was published online and Bid Opening and Evaluation Committees were appointed by the Additional Secretary and Health Secretary, respectively. Cabinet approval hadn’t been obtained. Bids were opened on the date the Cabinet finally gave the green light.
Sham evaluation
The Health Secretary appointed a five-member Evaluation Committee for these 285 medicines. There were no specialists or technical experts, and external input was not sought. Therefore, only prices and delivery times were considered—not the quality of supplies.
The Committee Chairman informed the Additional Secretary that, in some instances, evaluation couldn’t be carried out due to shortcomings in documents submitted by suppliers. The Additional Secretary instructed the Committee to select suitable parties based on delivery schedule and price. The non-availability of documents was a “major deviation” that was ignored by the Committee.
Owing to a backlog of unapproved registration applications at the National Medicines Regulatory Authority (NMRA) and other matters, there weren’t enough suppliers with valid licences for the required medicines. Therefore, many tenders were submitted without registration certificates as the Ministry had opened the doors—without restriction—to waivers of registration (WoRs) through this EoI process.
The “methodology which ensures the supply of medicines with quality had been deviated through relaxing the conditions,” the NAO holds.
Even where it granted WoRs, the NMRA violated the accepted methodology. Accordingly, the basic objective of providing medicines of high quality “is not fulfilled due to deviation from the responsibility on quality, safety and efficacy of such medicines”.
The EoI Evaluation Committee recommended that tenders be awarded (with WoRs) to all responsive suppliers, although they were not registered with the NMRA. By October 2022—in what was an unusually speedy process—the HSEPP had decided to hand out contracts for 170 medical items worth of US$ 19.8 million to the substantial responsive bidders.
“But the Procurement Committee had not taken measures to verify the quality of the medicines,” the NAO reiterates.
ICL deliberately left unused
The audit finds that a total of Rs. 2.9 billion of local funds were paid for direct medical procurements under this EoI method. Another Rs. 1.2 billion was due as of December last year.
To begin with, Indian manufacturers had been selected on the pretext of following the ICL procedure (with the Health Secretary even notifying 21 suppliers that their purchases would be through Indian credit). However, the ICL Subcommittee was set up under the Ministry’s Production, Supply and Regulation of Medicines Division headed by the errant Additional Secretary. And it did not submit the identified 159 orders worth US$ 19.1 million to the relevant parties.
The NAO states that “an opportunity was provided to avoid the implementation of these orders” under the ICL. Eventually, payments were made through local funds to handpicked Indian suppliers, restricting the opportunity for fair participation in the tender process and causing the purchase of medicines at higher prices. It also shut the doors to buying other quality medicines at a competitive price. The NAO says the Health Secretary’s actions caused losses to the government amidst a severe economic crisis.
A recommendation from the Deputy Director General of Medical Supplies and the errant Additional Secretary to—among other things—issue purchase orders without obtaining purchase agreements or performance securities and prior to obtaining Cabinet sanction was submitted to the then Health Minister on October 25, 2022. He approved it on the same day.
Waivers of registration
On approval of the Health Sector Emergency Procurement Committee, steps were taken to make emergency procurements worth Rs. 12.2 billion for 280 medicines through the State Pharmaceutical Corporation (SPC) between July 2022 and September 2023. Of these, WoRs were issued for 103 products.
But the Finance Minister (President Ranil Wickremesinghe), in his observations to a Cabinet memorandum that the then Health Minister had submitted, had clearly stated that when funds other than ICL are used, the Health Ministry must follow the relevant procurement guidelines. It did not sanction the EoI method that the Ministry was using.
Where WoRs were issued, the NMRA bypassed the usual method, which required submission of requests to a Waiver of Registration Subcommittee. Instead, waivers were granted by the NMRA Chief Executive Officer (CEO) through an unprecedented, fast-tracked “special pathway”.
Waivers were granted after merely checking documents such as purchase orders and sales invoices. No attention was given to elements such as price fairness; opinions of the relevant schools on medicine; essentiality of the medicine; existing number of similar registered medicines; registration conditions and status of the medicines; registration status of the supplier and the manufacturer; and prevailing prior issues on quality (quality failures), the NAO audit states. Documents related to quality, safety and efficacy were just not evaluated.
Despite Cabinet being told that a proper WoR process would be followed, “the Authority had deviated its own responsibility with regard to the quality of the medicines” by maintaining that the NMRA “had no responsibility for the medicines which fail in quality” and are imported through various schemes—including the ICL; that it was not answerable for their quality, safety and efficacy.
The NAO also highlights finger-pointing by the NMRA and the Health Ministry’s Medical Supplies Division (MSD). While the NMRA says the MSD is accountable for quality, safety and efficacy, the MSD Director has told the audit that the NMRA legally bears full responsibility regarding the issuance of WoRs.
|
In its strong recommendations, NAO calls for probe and legal action against those reponsible The audit recommends that investigations be carried out and legal action taken against the NMRA CEO, “who recommended the special pathway by bringing medicines to Sri Lanka without any minimum method to confirm the quality of the medicines and putting the patients at risk” as well as the NMRA Governing Board that approved it. If there is a need to exempt suppliers from registration in emergency situations, it is recommended that WoRs are issued in compliance with existing rules following verification of the quality of medicines. Regarding the call for EoIs and the procurement of medicines, including human immunoglobulin, on an unsolicited basis, the NAO calls for further investigations and legal action against those responsible for overriding Cabinet decisions; not doing technical evaluations properly; giving recommendations beneficial to suppliers; and prioritising two fake medications in making Companies and organisations that have supplied substandard medical products should promptly be blacklisted by the Finance Ministry, the Registrar of Companies and the Procurement Commission and prevented from resupplying medicines under other names. The NAO encouraged the NMRA to devise an efficient registration system that aligns with the government’s medical requirements. The quality of medicines must be maintained from the point of manufacture or import through regulation of government medicine stores and transportation. Medicines must be provided to the public at an affordable price by correcting deficiencies in pricing and regulation. The NAO proposes the establishment of an online computerised system linking agencies like the MSD, SPC, Customs and the Import and Export Control Department with the NMRA so that all documents—including registration and WoRs—can be cross-checked online. An accurate stock management system is recommended for reducing the lead time for obtaining medical supplies; forecasting the requirements of government hospitals and deciding reorder levels accurately; and maintaining a reliable, updated data system to enable timely submission of annual orders. The NAO states that delay charges must be imposed on suppliers that do not deliver on time. There must be frequent follow-up on orders and action taken in relation to orders that have less or no probability of being delivered. The audit proposes several other measures to ensure the smooth provision of medical supplies. If emergency purchases are deemed necessary even after taking those steps, and if such emergency purchases have been prompted by the negligence or inefficiency of officials, it recommends disciplinary action and the recovery of loss incurred by the government from the errant employees.
|
